Closing in on a cure
Colin Rensch fell in love with the piano when he was 11 years old. Seven years later, he got the chance to take a piano lesson from jazz legend Herbie Hancock, thanks to the Make-A-Wish Foundation.
Rensch was a percussionist in concert band at his high school in Mattawan, Michigan and then studied music history at Hope College in Holland, Michigan. Now 25 years old, he is finishing a master’s degree in history at Western Michigan University and applying to Ph.D. programs for musicology.
He also has Duchenne muscular dystrophy, the most common form of childhood-onset muscular dystrophy. When he was in high school, he began to lose strength in his arms and channeled his passion for music first into composing and then into studying the history of music.

“Knowing what I can and cannot do, that doesn’t really faze me very much. But it’s been a learning curve,” said Rensch, who has a number of assistants, sometimes up to 10, who help him throughout the day. “I first started with my assistants when I was in college, (and) I’ve learned a lot since then. I would say that coordinating with other people helping me is the most important thing.”
Duchenne, or DMD, is one of forms of muscular dystrophy, inherited diseases in which muscle tissue wastes away. DMD almost exclusively affects babies assigned male at birth, at an incidence of 1 in 3,500. Among muscular dystrophies, it is the most severe. Despite advances in cardiac and respiratory care that have allowed people with DMD to survive into adulthood, nearly all succumb to heart failure by their mid-30s.
DMD was first observed in the mid-19th century but was untreatable until corticosteroids were developed in the 1950s. For decades, steroids were the primary treatment for patients with DMD, along with drugs for secondary conditions that affect patients’ thyroid glands and lungs. That with the rollout of Sarepta Therapeutics’ Exondys 51, the brand name for eteplirsen, a drug that restores limited expression of the dystrophin protein by patching, or skipping, over the coding region of DNA called exon 51, which is missing in 13% of Duchenne patients. The drug, the Food and Drug Administration in 2016, is estimated to cost $300,000 per year.
But exon skipping is just one path forward for treating the disease. Each of the pharmaceutical companies Solid Biosciences, Pfizer and Sarepta has a drug candidate in clinical trials that delivers , a pared-down version of the massive gene that codes for dystrophin, to the muscles of people with DMD, where it is translated to make a mostly functional version of the dystrophin protein.
At the same time, studies in a handful of labs have shown promise in using the gene-editing machinery CRISPR–Cas9 to correct DMD-causing mutations in increasingly complex animal models. If researchers can find ways to subvert the human immune system’s response to the viral vectors that deliver CRISPR–Cas9 and can produce enough of those vectors to meet the needs of patients with DMD and other monogenetic disorders, they may be able to restore functioning fibers to the muscles and hearts of more than 300,000 people worldwide.
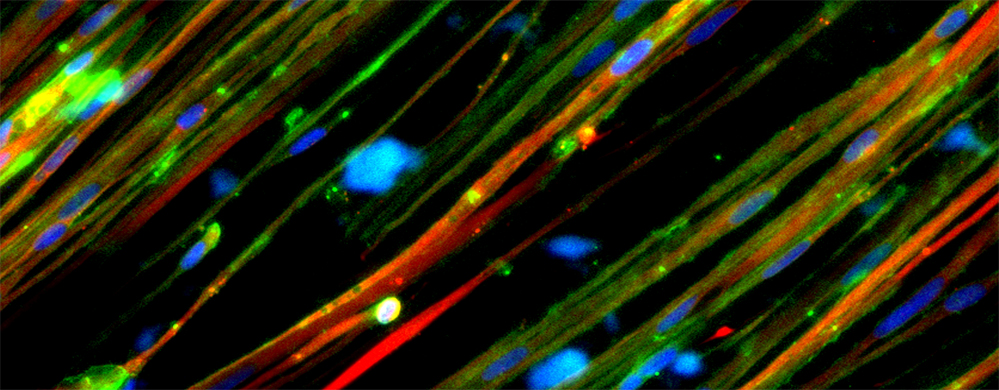
Faulty fibers
Situated beneath the cell membranes of striated muscle fiber cells, dystrophin proteins support muscle strength. In their absence, the muscle fibers’ actin and myosin contract and expand normally but the fibers are damaged more easily by routine activity.
Before children with DMD begin walking, their muscles generally don’t undergo enough strain to show wear. This means diagnoses are usually made when a child is 2 to 3 years old. Rensch said he was diagnosed when he was about 3.
During early childhood, however, the muscular stem cells that repair muscle by creating new tissue are extremely active and can compensate for and mask the damage being done, delaying a diagnosis until a child is age 7 or older.
is a neurologist at the University of Washington with expertise in muscular dystrophies.
“Early on in life, the boys do pretty well because there’s all this ongoing muscle cell damage, but then it’s repaired,” Chamberlain said. “The problems start occurring around age 4 or 5. Patients start losing muscle mass, and what’s thought to be happening is that this repair process just cannot keep up any longer.”
As the repair process fails, macrophages that produce cytokines infiltrate inflamed muscle cells. This causes both the formation of excess fibrous tissue and the emergence of fat cells within the muscle tissue.