Chronic fatty liver disease
Nonalcoholic fatty liver disease, or NAFLD, and its progressive form, nonalcoholic steatohepatitis, or NASH, have emerged as significant public health concerns in Western societies. NAFLD is a continuum of chronic fatty liver diseases ranging from benign hepatic steatosis to NASH, which consists of fatty liver with inflammation and injury. NASH can progress to severe fibrosis or cirrhosis, and primary hepatocellular cancer, . The increase in NAFLD in adults and children over the last 20 years parallels the obesity epidemic in Western societies. Factors contributing to the increased incidence of NAFLD include a sedentary lifestyle and poor diet of fat, simple sugar and cholesterol.
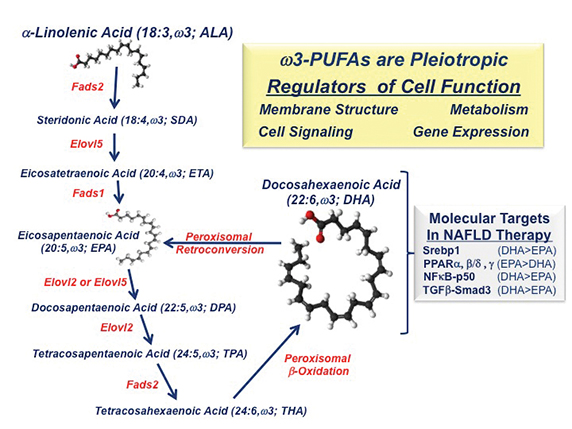 IMAGE COURTESY OF DONALD B. JUMP
IMAGE COURTESY OF DONALD B. JUMP
Since there are no U.S. Food and Drug Administration-approved drugs for NASH treatment, current therapies rely on lifestyle modification and treatment of the comorbidities associated with NAFLD, including obesity, hyperglycemia, dyslipidemia, hypertension and type 2 diabetes. Several clinical studies have evaluatedomega-3 fatty acids in , because omega-3 fatty acids have been reported to augment fatty-acid oxidation and triglyceride catabolism and suppress fatty-acid synthesis, inflammation and blood levels of triglycerides. Moreover, humans and mice with NAFLD have low hepatic omega-3 and omega-6polyunsaturated fatty acid, or PUFA content, when compared with healthy individuals (See and ).
Most clinical studies use a mix of eicosapentaenoic acid (20:5 EPA) and docosahexaenoic acid (22:6 DHA) and report that these dietary lipidslower liver fat but do not reduce , a risk factor for cirrhosis and HCC. In contrast, NAFLD patients consuming EPA have no reduction in . Studies of mice with NASH that lack the low-density lipoprotein receptor, or LDLR -/- have shown that DHA, but not EPA, reduces Western dietinduced fatty liver, inflammation and fibrosis (See and ).
The differential action of C20–22 omega-3 fatty acids on clinical outcomes can be explained, at least in part, by effects on fatty-acid metabolism and differences in the molecular actions of EPA versus DHA. DHA and EPA inhibit fatty-acid synthesis by suppressing the nuclear abundance of sterol regulatory element binding protein-1, a transcription factor controlling the expression of enzymes involved in de novo lipogenesis and PUFA synthesis. As such, humans and mice consuming EPA alone show no significant increase in blood or hepatic DHA content (See and ). DHA consumption, however, increases blood and hepatic DHA, EPA and the longchain n-3 fatty acid docosapentaenoic acid, or DPA. EPA and DPA increase .
Dietary DHA, but not EPA, attenuates Western diet-induced nuclear accumulation of transcription factors involved in inflammation, such as NF-kappa B, and fibrosis, such as phospho-Smad3. While NF-kappa B controls the expression of multiple inflammatory factors, including Cox2,chemokines and cytokines, phospho-Smad3 is a downstream mediator of TGF-beta signaling. TGF-beta is a major regulator of hepatic stellate . The impact of DHA on mouse liver fibrosis is TGF-beta receptors, factors regulating TGF-beta signaling, collagensubtypes, and enzymes involved in protein crosslinking and extracellular matrix remodeling.
Together, these studies establish that DHA controls several transcriptional regulatory networks relevant to NAFLD. There remain, however, several unanswered questions. Chief among these is determining why the mix of EPA and DHA fails to affect hepatic fibrosis in humans significantly. It will require more investigation to understand how omega-3 PUFA control pathways linked to chronic fatty liver disease.
Enjoy reading 91Ӱ��Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from 91Ӱ��Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

RA patient blood reveals joint innerworkings
Researchers in the Netherlands use mass spectrometry to compare the proteome of plasma and synovial fluid in rheumatoid arthritis patients and find a correlation. Read more about this recent paper in Molecular & Cellular Proteomics.

Hope for a cure hangs on research
Amid drastic proposed cuts to biomedical research, rare disease families like Hailey Adkisson’s fight for survival and hope. Without funding, science can’t “catch up” to help the patients who need it most.

Before we’ve lost what we can’t rebuild: Hope for prion disease
Sonia Vallabh and Eric Minikel, a husband-and-wife team racing to cure prion disease, helped develop ION717, an antisense oligonucleotide treatment now in clinical trials. Their mission is personal — and just getting started.

Defeating deletions and duplications
Promising therapeutics for chromosome 15 rare neurodevelopmental disorders, including Angelman syndrome, Dup15q syndrome and Prader–Willi syndrome.

Using 'nature’s mistakes' as a window into Lafora disease
After years of heartbreak, Lafora disease families are fueling glycogen storage research breakthroughs, helping develop therapies that may treat not only Lafora but other related neurological disorders.

Cracking cancer’s code through functional connections
A machine learning–derived protein cofunction network is transforming how scientists understand and uncover relationships between proteins in cancer.

