The quiet creep of Alzheimer鈥檚 disease
One day in 2001, Jodi Bottoni came home to find her clothes, shoes, money and small purple beaded lamp on the driveway. Her mother had thrown them out the front door of their home in Venice, Fla. Bottoni, who in her 40s had moved back in with her mother to care for her, was baffled. She assumed her mother, Jacquie Berg, was becoming an alcoholic and blamed scotch for the irrational behavior. But over the course of the next four years, Bottoni realized her mother’s increasingly erratic behavior, such as hoarding toilet paper in every nook and cranny of the house, couldn’t be attributed solely to alcohol. Something else was wrong. In 2005, Berg was diagnosed with Alzheimer’s disease.
Today, Bottoni is one of 15 million Americans who are caring for an Alzheimer’s patient at home. As of Brandeis University and Weill Cornell Medical College stated in his , caregivers are “the hidden victims” of the disease.
“I’ve put on tons of weight. I get no sleep. I’m stressed out,” says 54-year-old Bottoni, a bartender-waitress recovering from carpal tunnel surgery. “I have no life anymore. I don’t get to go anywhere. I don’t get to do anything. It’s terrible.”
Bottoni’s now 84-year-old mother, a former acrobat and Arthur Murray dance teacher whose features remind her daughter of the late actress Elizabeth Taylor, talks to her reflection in mirrors, incessantly hums and whistles, hides food in potted plants, and scribbles in coloring books with crayons. Her daughter has child-locked all doors leading out of the house and put a tracking bracelet on her mother’s ankle. During the night, Berg gets up four or five times to go to the bathroom. Bottoni’s 14-year-old Labrador, Morgan, sleeps in her mother’s room, and whenever the elderly woman rises out of bed, “he gets up and shakes his collar,” says Bottoni. “He lets me know she’s up and moving.” If Bottoni doesn’t catch her mother in time, she has to clean urine and feces from the floor, because her mother can no longer coordinate her movements and bodily functions.
So far, Bottoni has refused to put her mother, who adopted her as a child, in a nursing home. “I don’t trust anyone else to take care of her,” she says. “I love her to death. But I don’t know if I can do this anymore.”
The number of people in Bottoni’s shoes will rise if the disease goes unchecked. The global population is aging, and people in their mid-60s begin to become more susceptible to Alzheimer’s disease. By 2050, 100 million people around the world are projected to be stricken with the disease and 300 million people will become their caregivers.
Despite the potentially large number of victims of this fatal disease, Petsko has said, “I hear no clamor. I see no sense of urgency. If you knew an asteroid was going to hit the earth and would kill 100 million people, you would probably expect a worldwide clamor that something be done about it.”
The lack of public clamor, Petsko has argued, is at odds with the buzz of activity in Alzheimer’s disease research. Scientists are learning more about the molecular details of the disease and are optimistic that they may have drugs within the next five to 10 years to defend against its assault. But lack of public awareness of the disease’s impact means that there isn’t a push for faster research progress. “We’re grossly underspending on research for this field,” says of Weill Cornell Medical College, but “we’re facing an epidemic of unprecedented magnitude.”
Progression of Alzheimer's disease |
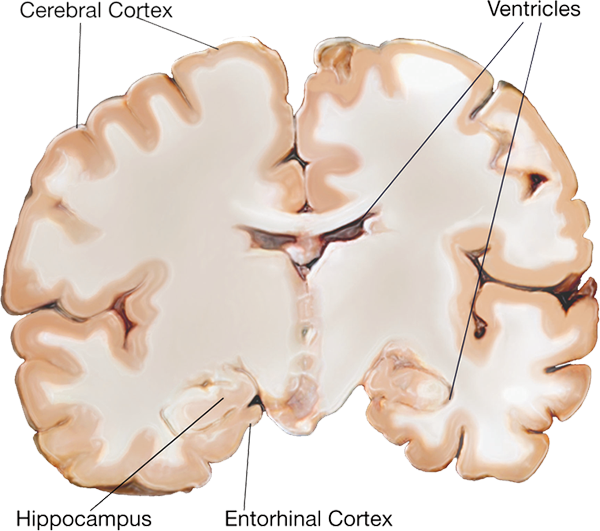 |
Healthy |
 |
Moderate |
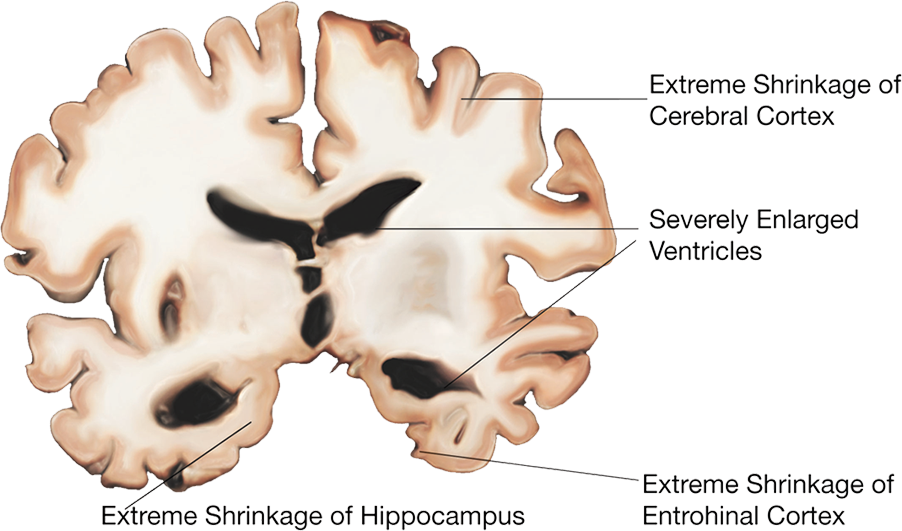 |
Severe |
Alzheimer’s disease is defined by two histopathological hallmarks in the brain, amyloid plaques and neurofibrillary tangles. These were first described more than a century ago by the Bavarian psychiatrist and neuropathologist Aloysius “Alois” Alzheimer. In 1901, Alzheimer met a 51-year-old female patient, Auguste Deter, at the Frankfurt Asylum. Deter showed strange behaviors, including screaming for hours in the middle of night, and experienced hallucinations. She had been admitted into the institution because her husband, a railroad worker named Karl, could no longer take care of her. Alzheimer became obsessed with her symptoms over the next few years. When Deter died in April 1906, Alzheimer acquired her medical records and brain. He used silver staining techniques to study her brain and later that year described at a conference the plaques and tangles he saw as well as her symptoms.
Alzheimer’s disease is mostly an age-related disorder, but “there’s been a longstanding debate (about) whether Alzheimer’s disease is an obligate consequence of aging,” says Relkin. There is evidence against that notion. Rare early-onset forms of the disease, based on autosomal dominant mutations, have been characterized in individuals who, like Deter, begin to display dementia by their 50s. These early-onset forms, which bear clinical and pathological similarities to the late-onset form, underscore that Alzheimer’s is a bona fide disease and not a foregone conclusion of aging.
The plaques, found outside of neurons, are now known to be clumps largely of a protein fragment called beta-amyloid or amyloid-beta. Aβ is a product of the proteolysis of a larger transmembrane protein called amyloid precursor protein. There are more than 30 types of Aβ fragments that differ in length, but the one that is found predominantly in plaques has 42 amino acids, Aβ42.
The neurofibrillary tangles are inside of neurons. They consist of a microtubule-associated protein called tau in a hyperphosphorylated form. When tau is not hyperphosphorylated, it stabilizes microtubules, which are important for maintaining cellular structure and acting as railroad tracks for the trafficking of various organelles. Tangles are seen in other types of dementia diseases, such as Pick’s disease, but in those cases they are not accompanied by plaques.
“There is some early indication that the amyloid, whether it’s aggregates or oligomers, triggers intracellular signaling pathways that involve tau and initiate the process of tangle formation,” says at the University of Toronto about Alzheimer’s disease. “But the exact mechanism hasn’t been completely figured out.”
 |
| Betty Wollslager. Photo provided by Eilene Wollslager. |
Eilene Wollslager recalls the moment when the enormity of her mother’s Alzheimer’s disease hit her. A professor of communications at the University of Texas, San Antonio, Wollslager had been watching her 85-year-old mother, Betty, lose her memory little by little over the course of seven years. In 2011, Wollslager had her parents move in with her and her husband so they could take over their care. But six months ago, when she walked into the kitchen, Wollslager was stunned. “My mom is a person who drinks 20 cups of coffee a day. She is a coffee addict. She was standing in front of the coffee maker and could not figure out how to make coffee,” Wollslager recalls. “That really hit me — just how far down the road we had come.”
Betty Wollslager was an elementary school teacher who taught third- and fourth-graders for 30 years. She was among the first generation in her family to go college. She was a voracious reader and was known as the family historian. But hints of the disease began to crop up in the mid-2000s. “She had been forgetful for a number of years. She wouldn’t remember little things. She couldn’t pull up a name or a word. She would go into rooms and forget why she was there,” says Eilene Wollslager. “You thought, ‘Oh well, she’s getting older.’ But it just kept going.”
When Betty Wollslager became aware that she was becoming forgetful, she began to keep a nightly journal in which she would record the day’s events. “At first, she could do it herself. Then she would have to ask Dad for help, because she couldn’t remember what happened in the day. Then she had to ask Dad pretty much for everything. Now she doesn’t do it,” says Eilene Wollslager.
These days, Betty Wollslager recognizes her husband and daughter but doesn’t remember her daughter’s name. “She cannot tell you where she lives. She can’t tell you what year it is and what day it is,” says Eilene Wollslager. “She lives totally in the moment.”
Alzheimer’s disease takes over the brain in a specific pattern. “It’s a $64,000 question of why certain cells die and others don’t,” says Petsko. “There is no question that the disease is focal. It starts in specific regions of the brain and spreads.”
The early stages of the disease ravage the entorhinal cortex, a region near the hippocampus. From there, it spreads to other parts of the limbic system, including the hippocampus, which is involved in emotions, behavior and long-term memory. The disease then invades the neocortical areas, at which point patients may begin to show disturbances in verbal fluency, orientation and copying geometric figures.
Autopsies reveal that plaques and tangles show up at different times. Plaques seem to appear anywhere from 20 to 30 years before symptoms. Neurofibrillary tangles seem more closely timed with the onset of disease symptoms but still precede them.
The thinking now is that oligomers of Aβ and tau, precursors to the plaques and neurofibrillary tangles, trigger neuronal death. Recent evidence suggests that tau can pass from cell to cell in a prionlike fashion, causing its normal counterparts in other cells to misfold and spur cell death.
of Banner Health Research says autopsies have shown that the brains of elderly people without Alzheimer’s can have plaques but no neurofibrillary tangles. The question is why, in some people, these plaques, after a certain load and time, trigger formation of neurofibrillary tangles and cause them to spread through the brain, bringing on clinical symptoms of Alzheimer’s.
The neuronal system isn’t the only one involved in the disease. Aβ and tau accumulation are thought to set off reactions involving glucose metabolism and inflammation. There are also links between insulin resistance and Alzheimer’s disease. at the National Institute on Aging explains that genetics has revealed hints of connections between the immune system and Alzheimer’s disease. “It fits that you might inherit a group of genes that make you a little more vulnerable to these protein aggregations because of your immune status,” he says.
Both Wollslager and Bottoni say it’s so hard to get their mothers to bathe that they attempt it only once a week. “It’s the weird things you battle over. My mom always was very fastidious. She always had every hair in place, crisp and clean,” says Wollslager. “We have a fight now every week about trying to get her to bathe. She thinks she’s already done it.”
Bottoni describes showering her mother as hell. “I have the heater in the

